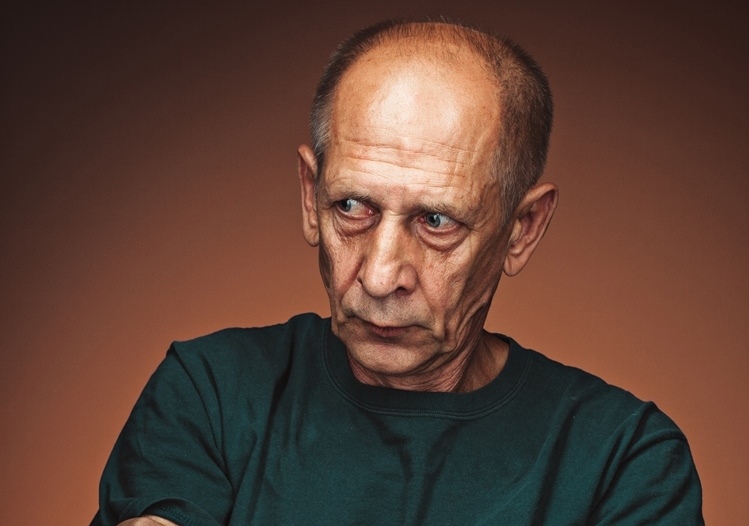
Parkinson’s Disease is a chronic, progressive neurodegenerative disorder of the brain that causes a gradual loss of muscle control. Age is the largest risk factor, with most people who develop Parkinson’s being 60 or older, and symptoms may take as long as 20 years to become full blown. While a small number of individuals are at risk because of a family history of the disorder, head trauma, exposure o environmental toxins, or illness could be risk factors.
Primary symptoms include slowness of movement, difficulty maintaining balance, muscle rigidity, and tremors. While there is no cure for Parkinson’s there are a number of treatment options available to make everyday life as easy as possible. Using a bath chair in the shower, well-lit stairwells, night lights for rooms and hallways, keeping walking areas clutter-free, avoiding rugs and/or carpets, and wearing low-heeled, comfortable shoes are some safety tips to keep in mind.
Worried that your loved or you might have Parkinson’s Disease?
- Does your loved one / you experience tremors or involuntary shaking of hands, arms, legs, jaw, and/or face?
- Does your loved one / you experience shuffling gait with short steps and trouble moving/walking?
- Does your loved one / you experience impaired balance and coordination?
- Does your loved one / you experience stiffness of the limbs and trunk?
- Does your loved one / you experience dizziness or frequent fainting?
- Does your loved one / you experience stooping or hunching over?
- Does your loved one / you experience slowness of movement?
- Does your loved one / you experience reduced arm swinging?
Treatments that can help your loved one or you:
Cognitive Behavioural Therapy (CBT)
Group Therapy